Macular edema following retinal vein occlusion
At a Glance










How It Affects You
Macular edema following retinal vein occlusion occurs when a blockage in the veins carrying blood away from the retina causes fluid to leak into the macula, the central part of the eye responsible for detailed vision. This fluid accumulation causes the macula to swell and thicken, leading to distorted or blurred eyesight. While the blockage itself happens in the blood vessels, the primary symptom is a painless change in vision that can range from mild blurring to severe visual impairment.
Key effects on the body include:
- Blurring or waviness of central vision
- Dark spots or missing patches in the visual field
- Potential for permanent vision loss if swelling persists untreated
Causes and Risk Factors
Underlying Causes
Macular edema following retinal vein occlusion develops due to a blockage in the veins that drain blood from the retina. When a retinal vein is blocked, pressure builds up within the capillaries, causing them to hemorrhage or leak fluid. This fluid accumulates in the macula, the center of the retina responsible for sharp, detailed vision. The blockage is often caused by the hardening of adjacent arteries which compress the vein, or by the formation of a blood clot (thrombus) within the vein itself.
Risk Factors
Several systemic health conditions increase the likelihood of developing retinal vein occlusion and subsequent macular edema. High blood pressure (hypertension) is the most significant risk factor. Other common contributors include high cholesterol, diabetes, and cardiovascular disease. Eye-specific conditions, such as glaucoma, can also increase risk by increasing pressure on retinal veins. Age is a primary factor, with the condition being rare in young people. Smoking and obesity are lifestyle factors that significantly elevate risk.
Prevention Strategies
Primary prevention focuses on managing the underlying risk factors that damage blood vessels. This involves maintaining healthy blood pressure and cholesterol levels, controlling diabetes, and quitting smoking. Regular comprehensive eye exams are crucial for detecting early signs of vascular changes or glaucoma. While there is no specific vaccine or guaranteed way to prevent a vein occlusion entirely, adopting a heart-healthy lifestyle with a balanced diet and regular exercise can support vascular health and reduce the probability of occurrence.
Diagnosis, Signs, and Symptoms
Signs and Symptoms
The most prominent symptom of macular edema following retinal vein occlusion is a painless blurring or distortion of central vision. Straight lines may appear wavy or bent, a symptom known as metamorphopsia. Colors may appear washed out or less vibrant. Symptoms can develop suddenly or gradually over days to weeks. Unlike some other eye conditions, peripheral (side) vision usually remains intact, although the occlusion itself can sometimes cause broader visual field defects. The severity of symptoms often correlates with the extent of the fluid leakage and whether the occlusion is in a branch vein or the central retinal vein.
Diagnostic Tests
Clinicians diagnose this condition through a comprehensive dilated eye examination. During the exam, the doctor looks for signs of bleeding, dilated veins, and swelling in the retina. Optical Coherence Tomography (OCT) is the gold standard for diagnosis; this non-invasive imaging test scans the retina to measure its thickness and visualize the fluid accumulation. Fluorescein angiography may also be performed, where a dye is injected into the arm to highlight blood flow and leakage in the retinal vessels. These tests help determine the severity of the edema and guide treatment decisions.
Differential Diagnosis
Doctors must distinguish this condition from other causes of macular edema and vision loss. It can be confused with diabetic macular edema, wet age-related macular degeneration, or macular edema resulting from ocular inflammation (uveitis). The specific pattern of hemorrhages and the appearance of the veins helps specialists differentiate retinal vein occlusion from these other disorders.
Treatment and Management
Medical Treatments
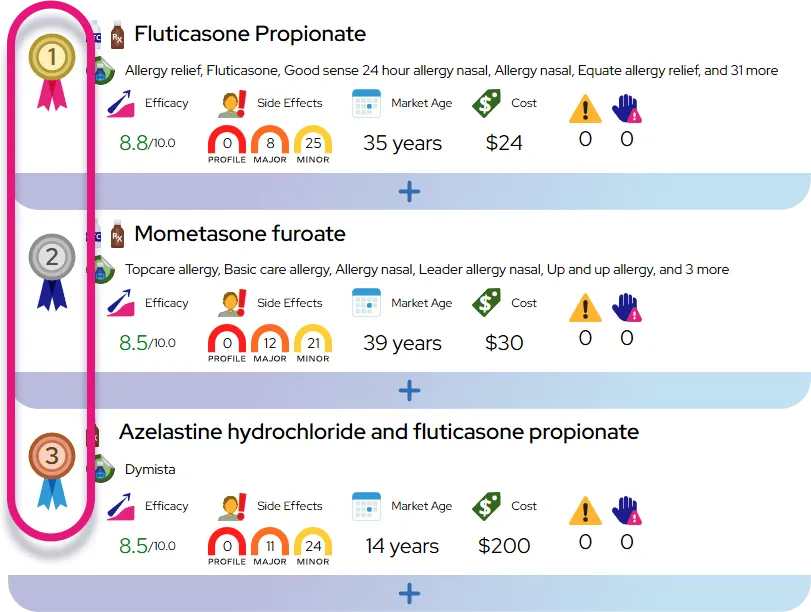
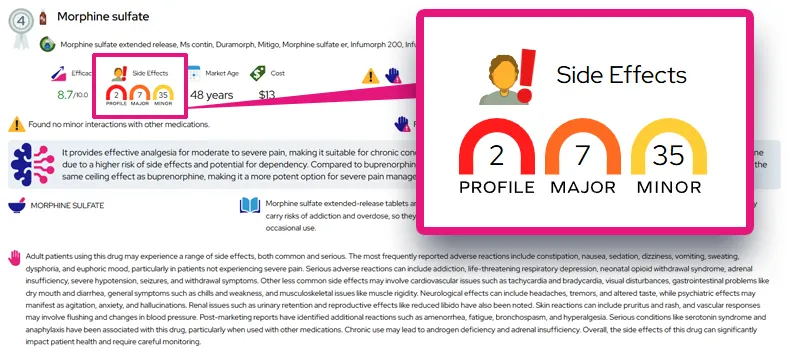
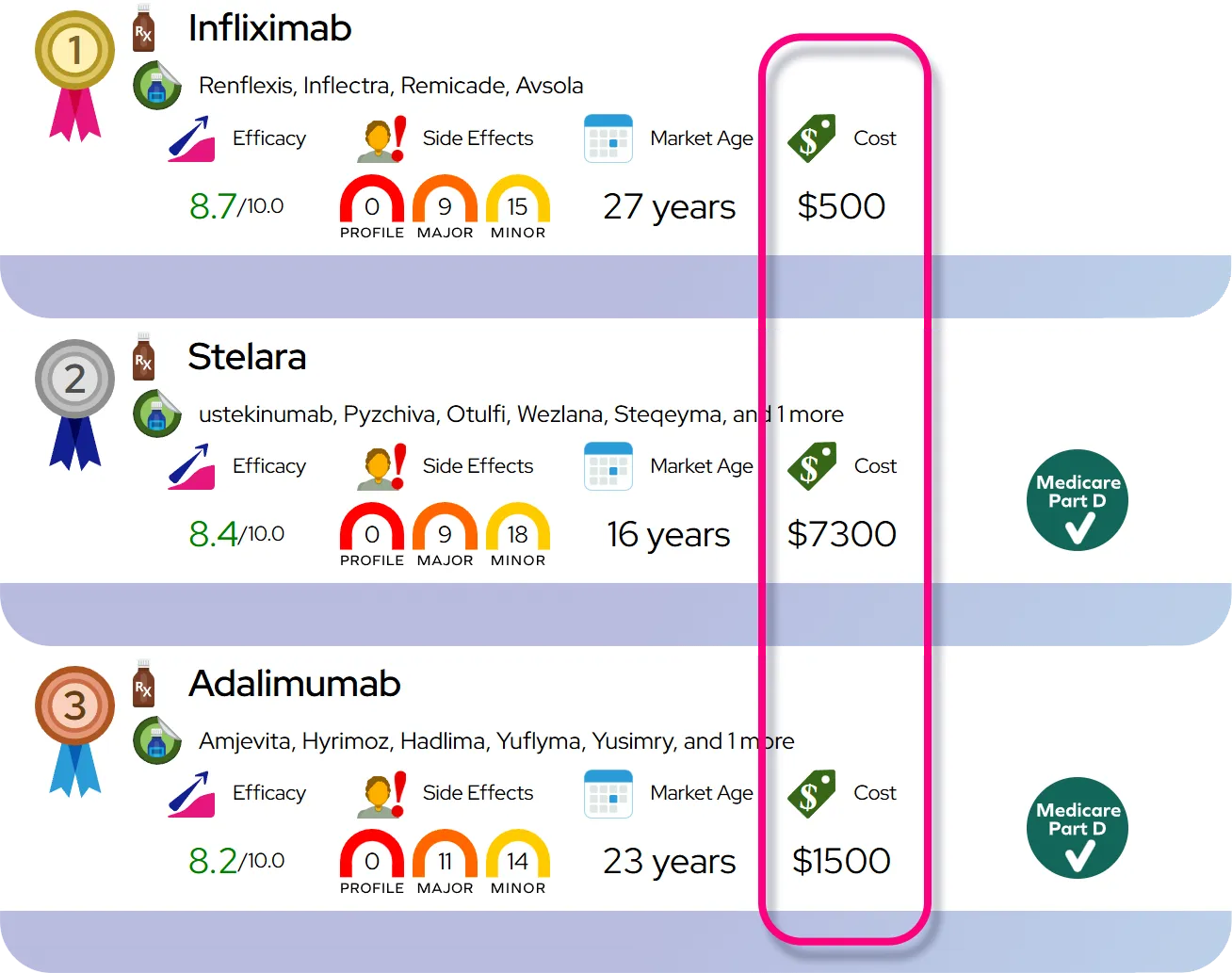
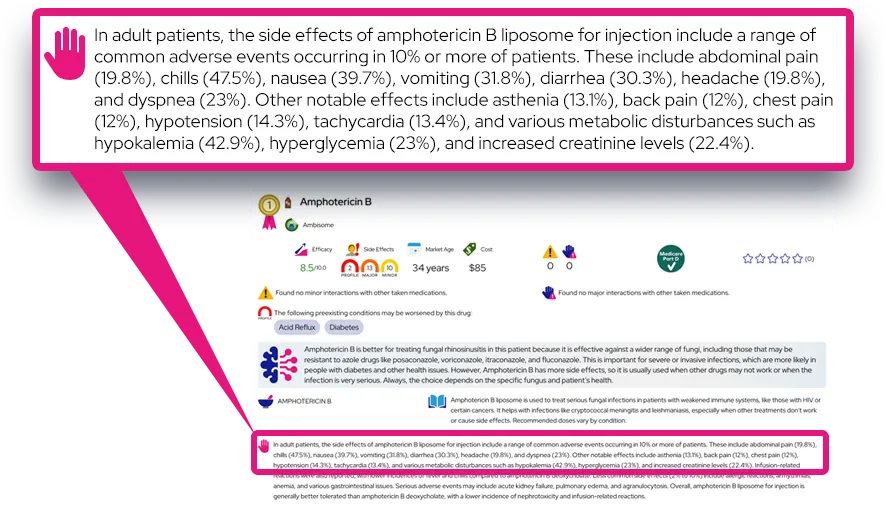
The primary goal of treatment is to reduce swelling and improve vision. The most common treatment involves intravitreal injections of anti-VEGF (vascular endothelial growth factor) medications. These drugs help stop the leakage of fluid from blood vessels and reduce swelling. Corticosteroid implants or injections are another effective option, particularly for patients who do not respond well to anti-VEGF therapy or for pseudophakic eyes (eyes with artificial lenses). Treatment is often ongoing, requiring repeated injections to maintain visual gains.
Laser Therapy
In some cases, focal or grid laser photocoagulation may be used to seal leaking blood vessels, particularly in cases involving branch retinal vein occlusion. While less common now as a first-line treatment due to the success of injections, it remains a useful tool in specific management plans. Pan-retinal photocoagulation may be necessary if abnormal new blood vessels begin to grow, preventing severe complications like glaucoma.
Management and Lifestyle
Managing the systemic conditions that contributed to the vein occlusion is a critical part of the overall care plan. Patients should work with their primary care providers to control blood pressure, cholesterol, and blood sugar levels. While lifestyle changes do not fix the existing eye damage directly, they prevent further vascular deterioration and protect the other eye.
When to Seek Medical Care
It is essential to seek immediate medical attention if there is a sudden change in vision, such as a drop in clarity, the appearance of new dark spots, or if straight lines suddenly look wavy. If pain or redness develops in the eye, this could signal a complication like high eye pressure and requires emergency care. Routine follow-up appointments are vital, as macular edema can recur even after successful treatment.
Severity and Prognosis
Severity and Complications
Macular edema following retinal vein occlusion can range from mild cases that resolve with minimal intervention to severe cases leading to legal blindness if untreated. The type of occlusion plays a role; Central Retinal Vein Occlusion (CRVO) generally presents more severe symptoms than Branch Retinal Vein Occlusion (BRVO). If the blockage prevents blood flow significantly (ischemic type), the risk of complications increases. Serious complications include the growth of abnormal, fragile blood vessels (neovascularization) which can bleed into the eye or cause neovascular glaucoma, a painful and vision-threatening type of high eye pressure.
Disease Course and Prognosis
The condition is typically chronic. While the initial vein blockage is an event, the resulting edema can persist or recur for years. Prognosis relies heavily on early detection and consistent treatment. With modern anti-VEGF therapy, many patients experience significant visual improvement and can maintain functional vision. However, some patients may have persistent fluid that is difficult to dry up completely. Visual acuity at the start of treatment is often a strong predictor of the final visual outcome.
Long-Term Health Risks
While the eye condition itself does not shorten life expectancy, it serves as a warning sign for systemic vascular health. Having a retinal vein occlusion indicates a higher risk for other vascular events, such as stroke or heart attack, emphasizing the need for comprehensive cardiovascular care. The risk of developing a vein occlusion in the fellow eye is relatively low but higher than in the general population.
Impact on Daily Life
Impact on Activities
Living with macular edema can make tasks requiring sharp central vision difficult. Reading, driving, recognizing faces, and watching television may become challenging due to blurred or distorted sight. Depth perception can be affected if one eye is significantly worse than the other, making activities like pouring liquids or navigating stairs trickier. Patients may need to rely more on their unaffected eye, which can lead to fatigue.
Coping Strategies
Using brighter lighting and high-contrast materials can help with reading and daily tasks. Magnifying devices or digital accessibility features (like increasing font size on phones) are practical tools. Ensuring the home environment is free of tripping hazards helps prevent falls if depth perception is compromised. Emotional support is also important, as vision loss can lead to anxiety or frustration.
Questions to Ask Your Healthcare Provider
Patients should feel empowered to ask questions to understand their care path. Consider asking the following:
- Is my condition ischemic or non-ischemic, and how does that affect my outlook?
- How frequently will I need injections, and for how long?
- What specific signs should prompt me to call you immediately between visits?
- Are there specific lifestyle changes I should prioritize to protect my other eye?
- Am I a candidate for laser treatment or steroid implants?
Common Questions and Answers
Q: Can macular edema following retinal vein occlusion be cured completely?
A: It is generally managed rather than cured. While the blocked vein may not reopen completely, treatment can effectively dry up the fluid in the macula and restore vision. Many patients require long-term monitoring and maintenance therapy to keep the swelling away.
Q: Will I go blind from this condition?
A: With modern treatments, total blindness is rare. Most patients retain or regain functional vision. However, if left untreated, severe swelling and complications like glaucoma can lead to significant and permanent vision loss in the affected eye.
Q: Does this condition affect both eyes?
A: It typically affects only one eye at a time. However, because the risk factors are systemic (like high blood pressure), there is a risk of it occurring in the other eye eventually. Controlling your overall health is the best way to protect both eyes.
Q: Are the eye injections painful?
A: The idea of an eye injection can be frightening, but the procedure is generally not painful. Doctors use numbing drops or gel to anesthetize the eye surface. Most patients report feeling pressure or a mild scratching sensation rather than sharp pain.
Q: Can I drive if I have this condition?
A: It depends on the severity of your vision loss and the laws in your region. If your other eye has good vision, you may still be legal to drive, but you should consult your eye doctor to ensure you meet the visual standards and are safe on the road.