Hypotension
At a Glance











How It Affects You
Hypotension, or low blood pressure, occurs when the force of blood flowing through the blood vessels is lower than expected, which can reduce the delivery of oxygen and nutrients to vital organs throughout the body. While often asymptomatic and considered a sign of good cardiovascular health in fit individuals, significant drops in pressure can compromise blood flow to the brain, heart, and other tissues. This lack of adequate perfusion can result in immediate physical instability or, in extreme cases, life-threatening shock.
Key effects on the body include:
- Insufficient blood flow to the brain leading to dizziness, lightheadedness, or fainting
- General weakness and fatigue due to reduced oxygen supply to muscles and tissues
- Potential organ damage if pressure drops low enough to cause shock
Causes and Risk Factors
Causes of Low Blood Pressure
Blood pressure is determined by how much blood the heart pumps and the amount of resistance to blood flow in the arteries. Hypotension can occur when the body cannot bring blood pressure back to normal ranges quickly enough. Several biological mechanisms and conditions can cause this drop. Dehydration is a common cause, as losing more water than is taken in reduces blood volume. Heart problems, such as an extremely low heart rate (bradycardia), heart valve problems, or heart failure, can prevent the heart from pumping enough blood. Endocrine problems, including thyroid conditions, adrenal insufficiency (Addison's disease), and low blood sugar, may also interfere with blood pressure regulation. Severe infections can lead to septic shock, a dangerous form of hypotension. Additionally, significant blood loss from an injury or internal bleeding reduces the amount of blood in the circulatory system, leading to a severe drop in pressure. Severe allergic reactions (anaphylaxis) can also cause blood pressure to plummet.
Risk Factors and Triggers
Certain factors increase the likelihood of developing low blood pressure. Age is a significant factor; older adults are more prone to orthostatic hypotension (dropping pressure when standing) and postprandial hypotension (dropping pressure after eating), while children and young adults are more likely to experience neurally mediated hypotension. Certain medications are known triggers, including diuretics (water pills), alpha blockers, beta blockers, drugs for Parkinson's disease, and some antidepressants. People with specific diseases, such as diabetes, Parkinson's disease, and some heart conditions, are at higher risk. Pregnancy can also cause hypotension because the circulatory system expands rapidly, though this usually resolves after giving birth. Triggers for episodes can include standing up too quickly, standing for long periods, extreme heat, or large meals.
Prevention Strategies
Preventing symptomatic hypotension often involves lifestyle adjustments to maintain stable blood pressure. Primary prevention focuses on staying well-hydrated and maintaining a balanced diet with adequate nutrients like vitamin B12 and folate, as deficiencies can cause anemia and low blood pressure. Strategies to reduce flare-ups include avoiding alcohol, which can dehydrate the body, and rising slowly from sitting or lying down positions to prevent dizziness. For those with postprandial hypotension, eating smaller, lower-carbohydrate meals can help. Wearing compression stockings may improve blood flow from the legs to the heart. It is not always possible to prevent hypotension caused by genetic factors or unavoidable medical treatments, but managing the risk factors can significantly reduce the frequency of symptoms.
Diagnosis, Signs, and Symptoms
Signs and Symptoms
For many people, low blood pressure causes no noticeable symptoms and requires no intervention. However, when blood pressure drops low enough to impair oxygen delivery to the body, symptoms appear. The most common early signs include dizziness or lightheadedness, particularly when changing positions. Other frequent symptoms involve fainting (syncope), blurred or fading vision, nausea, fatigue, and a lack of concentration. In severe cases linked to shock, symptoms become more critical and include confusion, cold or clammy pale skin, rapid shallow breathing, and a weak and rapid pulse. Symptoms can vary by population; for example, older adults may primarily experience falls or unsteadiness upon standing, while younger individuals might faint after standing for long periods.
How Hypotension is Diagnosed
Clinicians identify hypotension primarily through blood pressure measurement using an inflatable cuff. A reading lower than 90 millimeters of mercury (mm Hg) for the top number (systolic) or 60 mm Hg for the bottom number (diastolic) is generally considered low. To understand the underlying cause and type of hypotension, doctors may perform additional tests. Blood tests can check for low blood sugar, high blood sugar (diabetes), or a low red blood cell count (anemia). An electrocardiogram (ECG) detects irregularities in heart rhythm, while an echocardiogram examines heart function and structure. A stress test measures how the heart performs during physical activity. A tilt table test is often used for people who faint for unknown reasons; this evaluates how the body reacts to changes in position. Doctors also consider differential diagnoses, ensuring the symptoms are not caused by vertigo, inner ear problems, anxiety, or isolated hypoglycemia, which can mimic the dizziness associated with hypotension.
Treatment and Management
Treatment and Management Strategies
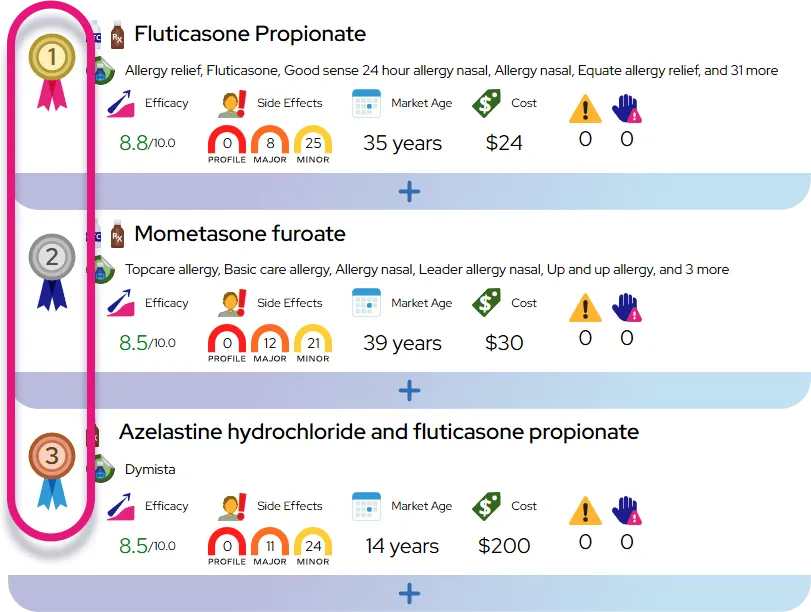
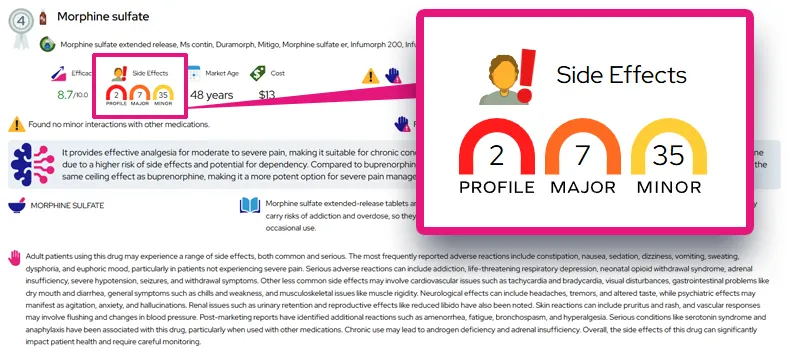
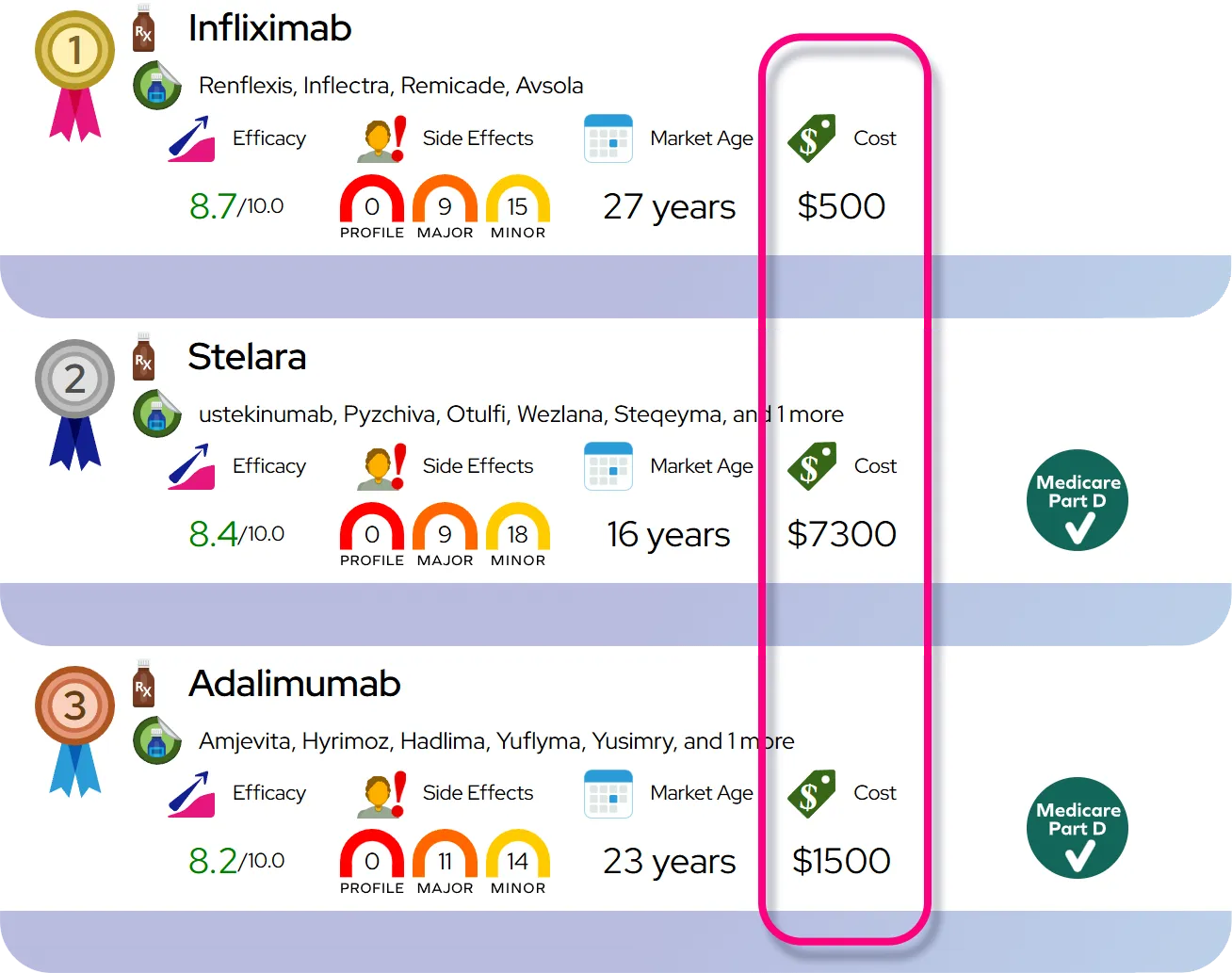
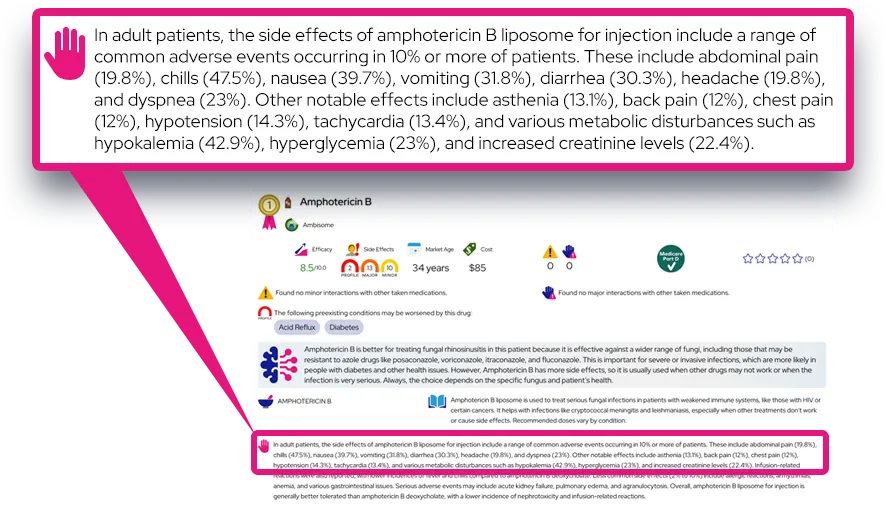
Treatment for hypotension depends on the underlying cause and the severity of symptoms. If low blood pressure is asymptomatic, it generally does not require treatment. When symptoms are present, the goal is to raise blood pressure to a safe level and address the root cause. If medications are the culprit, a doctor may adjust the dosage or switch to a different drug. For persistent types of hypotension, medications such as fludrocortisone may be prescribed to boost blood volume, or midodrine to restrict the ability of blood vessels to expand, thereby raising pressure. These treatments address the physiological mechanisms to improve symptoms. Effectiveness varies; lifestyle changes work well for mild cases, while medication is often necessary for neurogenic orthostatic hypotension.
Lifestyle and Self-Care
Lifestyle modifications are often the first line of defense. Drinking plenty of water prevents dehydration and increases blood volume. Unlike the advice for high blood pressure, increasing salt intake can be beneficial for those with hypotension, as sodium helps raise blood pressure; however, this should only be done under medical supervision. Wearing compression stockings covering the calves and thighs can reduce the pooling of blood in the legs. Physical maneuvers, such as crossing the legs while sitting or tensing leg muscles before standing, can help pump blood back to the heart. Avoiding heavy lifting, hot showers, and standing still for long periods can also reduce the risk of fainting.
When to Seek Medical Care
Routine follow-up is important for monitoring the effectiveness of treatment, but immediate care is sometimes necessary. Patients should see a doctor if they experience frequent dizziness or fainting episodes. Emergency medical care should be sought if signs of shock appear, such as cold and clammy skin, rapid shallow breathing, a weak and rapid pulse, or confusion. Sudden or severe symptoms, especially if accompanied by chest pain, shortness of breath, or a high fever, require urgent evaluation. It is important to discuss any falls or injuries resulting from dizziness with a healthcare provider.
Severity and Prognosis
Severity and Disease Course
Hypotension ranges from a mild, asymptomatic variance in normal physiology to a severe, life-threatening condition. Mild hypotension is often seen in fit individuals and is generally harmless. Moderate cases may involve recurrent dizziness or fainting that interferes with daily activities. Severe hypotension can lead to shock, a medical emergency where organs do not get enough blood. The course of the condition depends on the cause. Acute hypotension caused by dehydration or blood loss is temporary and resolves once the volume is restored. Chronic forms, such as those related to nervous system disorders, may require lifelong management. Symptoms can fluctuate, often worsening with heat, dehydration, or after meals.
Complications and Long-Term Effects
The primary complication of hypotension is fall-related injury. Dizziness and fainting can lead to broken bones, concussions, or other trauma, particularly in older adults. Long-term, if blood pressure remains critically low, it can deprive the heart and brain of oxygen, potentially leading to heart damage or stroke-like complications, although this is less common than with high blood pressure. Severe, prolonged shock can result in permanent organ failure, such as kidney damage. However, for most people with chronic, mild low blood pressure, there are no negative long-term effects on other organs.
Prognosis
The overall prognosis for hypotension is generally good. When caused by treatable factors like dehydration or medication side effects, the condition can be completely resolved. For chronic conditions like orthostatic hypotension, symptoms can usually be effectively managed with lifestyle changes and medication, allowing for a normal quality of life. Life expectancy is typically not reduced by hypotension itself, except in cases where it is a marker for severe frailty or advanced heart disease. Early diagnosis and consistent management of triggers are key factors that positively influence the outcome.
Impact on Daily Life
Daily Activities and Coping
Living with symptomatic hypotension requires mindfulness about physical movements and daily habits. Activities that involve rapid changes in posture, such as getting out of bed or standing up from a chair, must be done slowly to avoid dizziness. Some people may need to sit down in the shower or avoid hot environments like saunas, which can dilate blood vessels and lower pressure further. Socially, individuals might feel self-conscious about the need to sit or lie down suddenly if they feel faint. Functionally, fatigue can limit stamina for work or exercise. Practical coping strategies include eating small, low-carb meals to prevent post-meal crashes and keeping water available at all times. Mental health can be impacted by the fear of fainting in public or the frustration of physical limitations, so finding a support network or speaking with a counselor can be helpful.
Questions to Ask Your Healthcare Provider
To better understand the condition and how to manage it, patients should consider asking the following questions at their next appointment:
- What is the most likely cause of my low blood pressure?
- Are any of my current medications contributing to my symptoms?
- How much salt and water should I be consuming each day?
- What specific signs indicate that I need to seek emergency care?
- Are there specific exercises that are safe and beneficial for me?
- Should I monitor my blood pressure at home, and if so, how often?
- What should I do if I feel like I am about to faint?
Common Questions and Answers
Q: What blood pressure reading is considered too low?
A: Generally, a blood pressure reading lower than 90/60 mm Hg is considered hypotension. However, doctors usually only consider it a problem if it causes symptoms like dizziness, fainting, or fatigue.
Q: Can drinking coffee help with low blood pressure?
A: Caffeinated beverages like coffee can temporarily raise blood pressure by stimulating the cardiovascular system. Some doctors may suggest a cup of coffee with meals for certain patients, but it is important to balance this with water to avoid dehydration.
Q: Is low blood pressure as dangerous as high blood pressure?
A: Typically, chronic low blood pressure is not as dangerous as high blood pressure and does not carry the same risks for heart attack and stroke. However, sudden drops in blood pressure can be dangerous if they lead to falls, injuries, or shock.
Q: Why do I feel dizzy when I stand up?
A: This is likely due to orthostatic hypotension. When you stand, gravity pulls blood into your legs. If your body does not adjust quickly enough by constricting blood vessels and increasing heart rate, your blood pressure drops, causing temporary dizziness.
Q: Can I exercise if I have hypotension?
A: Yes, exercise is generally beneficial as it promotes blood flow. However, you should avoid exercises that involve sudden changes in head position or holding your breath. It is best to warm up slowly and stay hydrated. Consult your doctor for a safe exercise plan.