Hypertension
At a Glance











How It Affects You
Hypertension places excessive strain on the body's arteries, forcing the heart to pump harder than necessary to circulate blood effectively. Over time, this continuous high pressure can damage the inner lining of arteries throughout the entire body, leading to plaque buildup that narrows the vessels and restricts blood flow. Without management, this systemic damage significantly increases the workload on vital organs and can lead to serious health events.
- Increases the risk of life-threatening conditions such as heart attack and stroke.
- Damages the delicate blood vessels in the kidneys and eyes, potentially leading to organ failure or vision loss.
- Contributes to the hardening and thickening of arteries, reducing the efficiency of oxygen delivery to tissues.
Causes and Risk Factors
Understanding the Causes
For most adults, there is no single identifiable cause of high blood pressure. This type is known as primary or essential hypertension and it tends to develop gradually over many years due to a complex interaction of genetics and environment. In a smaller number of cases, known as secondary hypertension, the condition is caused by an underlying condition such as kidney disease, adrenal gland tumors, thyroid problems, obstructive sleep apnea, or certain congenital heart defects. Some medications, including birth control pills, cold remedies, decongestants, and over-the-counter pain relievers, can also lead to secondary hypertension.
Risk Factors and Triggers
Various factors increase the likelihood of developing high blood pressure. Some risk factors are not modifiable, such as family history, age, and race; for example, high blood pressure is more common among African American adults and often develops at an earlier age. Modifiable risk factors related to lifestyle play a major role in the development of the condition.
- Being overweight or obese requires more blood to supply oxygen and nutrients to tissues.
- Physical inactivity tends to increase heart rate and force the heart to work harder.
- Diets high in sodium causing the body to retain fluid.
- Diets low in potassium which helps balance the amount of sodium in cells.
- Tobacco use which immediately raises blood pressure and damages blood vessel walls.
- Drinking too much alcohol which can damage the heart over time.
- High levels of stress which can lead to temporary but dramatic increases in blood pressure.
Prevention Strategies
Primary prevention focuses on adopting a heart-healthy lifestyle to stop high blood pressure from developing in the first place. This includes maintaining a healthy weight, eating a balanced diet rich in fruits and vegetables, limiting salt intake, exercising regularly, and managing stress. For those who already have the condition, these same steps are crucial for preventing the disease from worsening and avoiding complications. Monitoring blood pressure at home and keeping regular medical appointments are also key preventive measures against severe health events.
Diagnosis, Signs, and Symptoms
Common Signs and Symptoms
Hypertension is often called the "silent killer" because most people with high blood pressure have no signs or symptoms, even when blood pressure readings reach dangerously high levels. A person can have high blood pressure for years without knowing it. In rare cases where blood pressure is extremely high, individuals may experience specific symptoms, though these are not reliable indicators for early diagnosis.
- Severe headaches
- Shortness of breath
- Nosebleeds
- Flushing or dizziness
- Chest pain
- Visual changes
How Clinicians Identify the Condition
The only way to detect hypertension is to have blood pressure measured. This is a quick and painless test using a pressure cuff placed around the arm. A healthcare provider will typically diagnose hypertension if the average of two or more blood pressure readings on two or more separate occasions indicates high pressure. Blood pressure is recorded as two numbers: systolic pressure (the top number, measuring pressure when the heart beats) and diastolic pressure (the bottom number, measuring pressure when the heart rests between beats). Clinicians may also recommend home monitoring or a 24-hour ambulatory blood pressure monitor to confirm the diagnosis and rule out "white coat hypertension," where blood pressure is only high in a medical setting.
Additional Testing and Differential Diagnosis
Once diagnosed, doctors may order additional tests to check for signs of heart disease or kidney damage, or to look for underlying causes. These tests often include a urinalysis, blood tests to measure cholesterol and potassium levels, and an electrocardiogram (ECG or EKG) to measure the heart's electrical activity. Differential diagnosis involves ruling out other conditions that might mimic symptoms or cause temporary spikes in blood pressure, such as anxiety disorders, acute pain, or substance withdrawal.
Treatment and Management
Lifestyle and Self-Care Strategies
The first line of defense in managing hypertension is often changing one's lifestyle. These changes can be very effective at lowering blood pressure and may reduce the need for medication. Key strategies include eating a heart-healthy diet with less salt (often referred to as the DASH diet), getting regular physical activity, maintaining a healthy weight, and limiting the amount of alcohol consumed. Quitting smoking is also essential, as it helps reduce the risk of heart disease and improves overall vascular health. Stress management techniques, such as deep breathing, meditation, and muscle relaxation, can also help stabilize blood pressure levels.
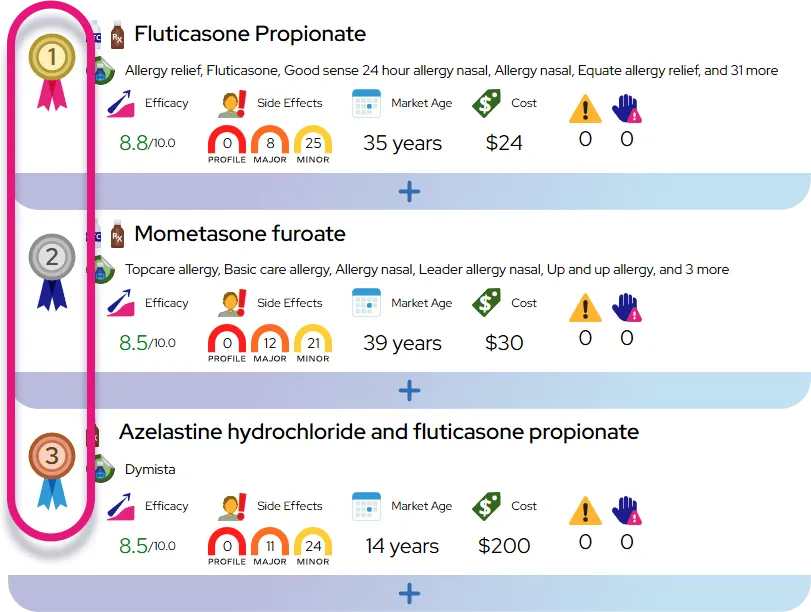
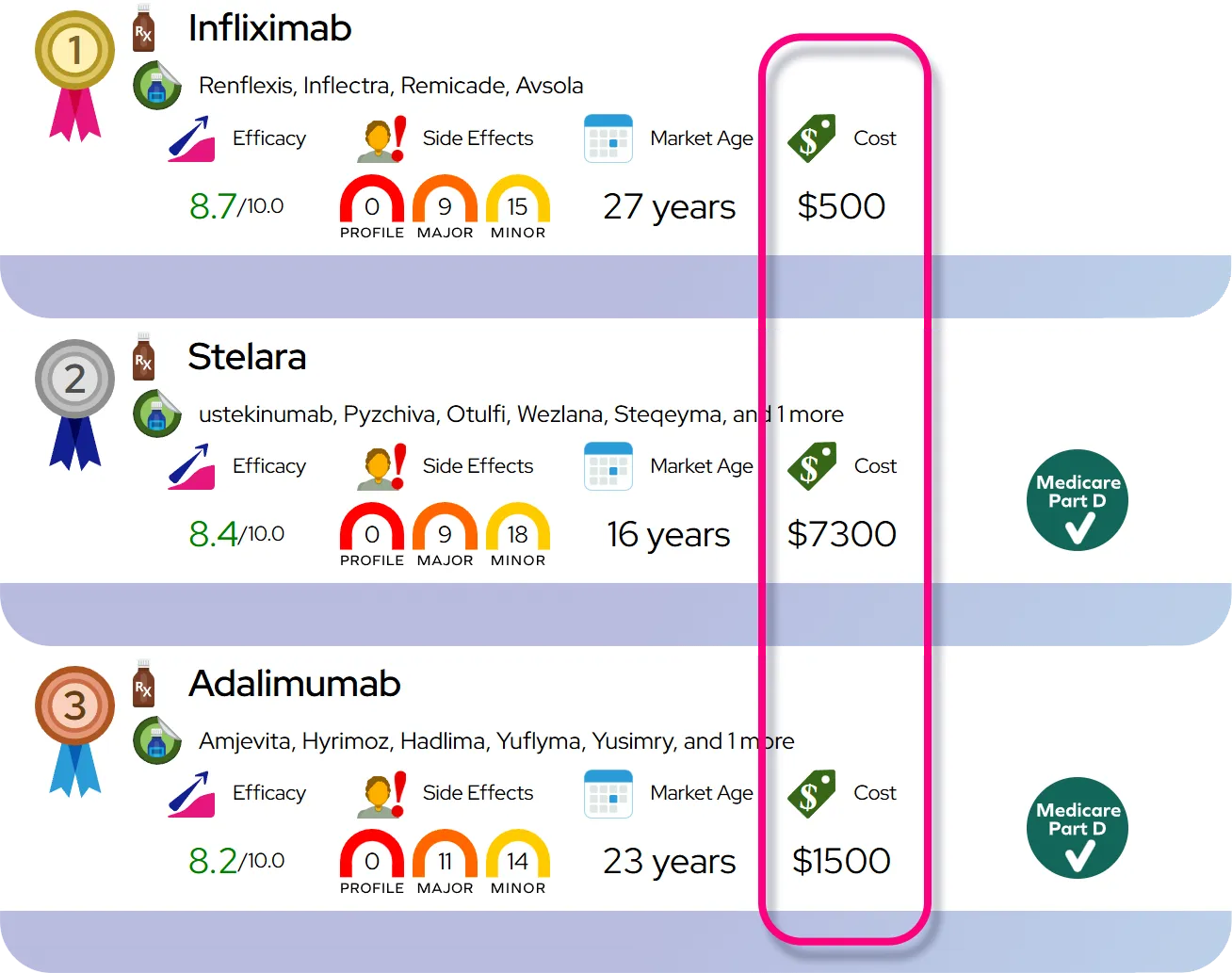
Medications
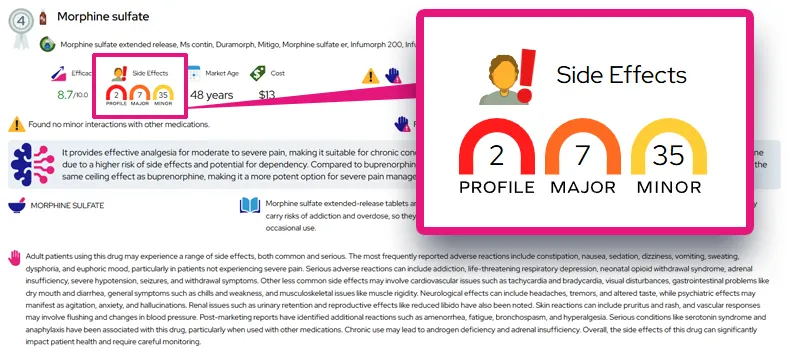
When lifestyle changes alone are not enough, healthcare providers may prescribe medication. There are several types of blood pressure medications, and they work in different ways to lower pressure. It is common to need a combination of medications to reach treatment goals. Taking these medications exactly as prescribed is critical for them to work effectively.
- Diuretics (water pills) help kidneys eliminate sodium and water.
- Angiotensin-converting enzyme (ACE) inhibitors help relax blood vessels.
- Angiotensin II receptor blockers (ARBs) relax blood vessels by blocking a chemical that narrows them.
- Calcium channel blockers prevent calcium from entering heart and vessel muscle cells, allowing relaxation.
- Beta-blockers reduce the workload on the heart and open blood vessels.
When to See a Doctor
Routine follow-up is necessary to monitor blood pressure levels and adjust medications. Immediate medical care is required if blood pressure readings are sudden and significantly higher than normal, especially if accompanied by concerning symptoms. Red-flag symptoms that warrant emergency care include severe chest pain, severe headache accompanied by confusion or blurred vision, numbness or weakness on one side of the body, or difficulty breathing. These could be signs of a hypertensive crisis, heart attack, or stroke.
Severity and Prognosis
Severity Levels
Hypertension is categorized into stages based on the severity of the pressure readings. It ranges from elevated blood pressure, which is a warning sign, to Stage 1 and Stage 2 hypertension, where the risk of damage increases. A hypertensive crisis is a severe increase in blood pressure that can lead to a stroke. The condition is generally considered more serious if it is resistant to treatment or if other risk factors like diabetes or high cholesterol are present. While the condition typically starts as mild, without intervention it tends to progress and become more severe over time.
Complications and Long-Term Effects
The long-term prognosis depends heavily on how well the blood pressure is controlled. Uncontrolled high blood pressure can lead to severe complications by damaging the arteries and decreasing blood flow to the heart and other organs. These complications can disable patients or be fatal. Hardened arteries, or atherosclerosis, can lead to heart attack and stroke. The heart muscle may thicken and eventually fail to pump enough blood to meet the body's needs (heart failure). Other organ systems are also at risk; blood vessels in the kidneys can weaken and narrow, preventing proper function, while damage to eye blood vessels can result in vision loss.
Factors Influencing Prognosis
For the vast majority of people, hypertension is a manageable condition rather than a fatal one, provided they adhere to treatment plans. Early diagnosis significantly improves the outlook because it allows for intervention before permanent organ damage occurs. Patients who maintain a healthy lifestyle and take prescribed medications typically have a good prognosis and can expect a normal lifespan. Conversely, ignoring the condition increases the risk of premature death from cardiovascular events.
Impact on Daily Life
Impact on Daily Activities and Emotional Health
Living with hypertension often requires making permanent adjustments to daily routines, particularly regarding diet and exercise. This can initially feel burdensome or restrictive. Grocery shopping and cooking may take longer as patients learn to read labels for sodium content and prepare fresh meals. Some blood pressure medications may cause side effects like fatigue, frequent urination, or dizziness, which can temporarily affect work or social activities until the right dosage is found. A diagnosis can also bring anxiety or stress regarding potential health risks, creating a cycle that needs management since stress itself can raise blood pressure. However, many people find that the healthy lifestyle changes adopted for hypertension lead to increased energy and better overall well-being in the long run.
Questions to Ask Your Healthcare Provider
Being prepared for medical appointments helps ensure that patients understand their condition and care plan. Patients should consider bringing a list of questions to discuss with their doctor.
- What is my target blood pressure number?
- How often should I check my blood pressure at home?
- What specific diet or exercise changes do you recommend for me?
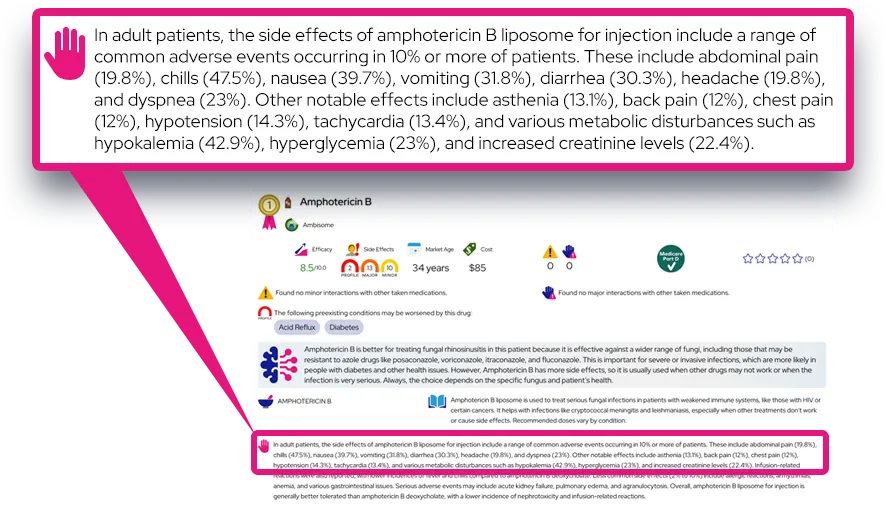
- What are the potential side effects of my prescribed medication?
- Is my blood pressure high enough to damage my organs?
- What should I do if I miss a dose of my medication?
- At what blood pressure reading should I seek emergency care?
Common Questions and Answers
Q: Can I stop taking my medication if my blood pressure goes down?
A: No, you should not stop taking your medication without consulting your doctor. Normal readings usually mean the medication is working, not that the hypertension is cured. Stopping suddenly can cause your blood pressure to spike again.
Q: Is sea salt better for me than table salt?
A: Generally, no. Sea salt and table salt have roughly the same amount of sodium by weight. To lower blood pressure, it is necessary to limit total sodium intake regardless of the source.
Q: Can I feel when my blood pressure is high?
A: Most of the time, you cannot feel high blood pressure. It typically does not cause symptoms like headaches or sweating unless it is in a dangerously high range (hypertensive crisis). The only way to know for sure is to measure it.
Q: Does drinking coffee cause hypertension?
A: Caffeine can cause a short, temporary spike in blood pressure, but it is not clear if it causes long-term hypertension. Doctors may advise limiting caffeine if you are sensitive to it or if it affects your specific readings.
Q: Is high blood pressure curable?
A: For most people, hypertension is a chronic condition that is managed rather than cured. However, in some cases where it is caused by another medical condition (secondary hypertension), treating the underlying problem may resolve the high blood pressure.