Cataplexy
At a Glance











How It Affects You
Cataplexy causes a sudden and temporary loss of voluntary muscle tone while a person is awake, ranging from subtle weakness to total collapse. The episodes are typically triggered by strong emotions such as laughter, excitement, or anger, and can affect specific muscle groups or the entire body. Unlike fainting or seizures, consciousness remains fully intact throughout the episode.
- Involves weakness in the face, neck, knees, or the entire skeletal muscle system
- Preserves awareness and memory of the event while it happens
- Varies in duration from a few seconds to several minutes
Causes and Risk Factors
Underlying Causes
Cataplexy is caused by the loss of specific neurons in the brain (hypothalamus) that produce hypocretin (also known as orexin), a chemical that helps regulate wakefulness and muscle tone. In almost all cases, this loss is believed to be the result of an autoimmune reaction where the body's immune system mistakenly attacks these healthy cells. While the exact trigger for this immune attack is unknown, it may be influenced by a combination of genetic predisposition and environmental factors, such as infections.
Common Triggers
Episodes of cataplexy are uniquely precipitated by strong, sudden emotions. Positive emotions are the most common triggers, but negative emotions can also cause attacks. Triggers vary significantly between individuals.
- Laughter and joking (the most common trigger)
- Excitement or pleasant surprise
- Anger, frustration, or annoyance
- Fear or stress
Risk Factors
The primary risk factor for developing cataplexy is having Type 1 Narcolepsy. Other factors that increase the likelihood of developing the condition include specific genetic markers (such as the HLA-DQB1*06:02 gene) and a family history of narcolepsy, although it rarely runs directly in families. Rarely, cataplexy can be caused by secondary medical conditions that damage the brain, such as tumors, Niemann-Pick type C disease, or strokes.
Prevention
There is currently no known way to prevent the underlying loss of hypocretin cells that causes the condition to develop. Primary prevention strategies such as vaccines or screenings do not exist for the condition itself. However, once diagnosed, patients can prevent individual attacks by managing known emotional triggers and adhering to their treatment plan.
Diagnosis, Signs, and Symptoms
Signs and Symptoms
Cataplexy is characterized by muscle weakness that occurs while a person is fully conscious. The severity can range from mild, barely noticeable symptoms to severe episodes resulting in physical collapse. Symptoms usually last from a few seconds to a couple of minutes, and muscle tone returns to normal immediately afterward. Importantly, the person remains awake, can hear, and is aware of their surroundings throughout the episode.
- Facial Weakness: Drooping eyelids, sagging jaw, or flickering facial muscles.
- Speech Issues: Slurred speech or inability to speak despite trying.
- Body Weakness: Head dropping, shoulders slumping, buckling of the knees, or dropping objects held in the hands.
- Total Collapse: Complete loss of muscle tone leading to a fall, though breathing and eye movements are unaffected.
Diagnosis
Clinicians diagnose cataplexy primarily through a detailed medical history, specifically looking for the link between emotional triggers and muscle weakness. Because cataplexy is almost exclusive to Type 1 Narcolepsy, verifying its presence is key to diagnosis. Several tests confirm the diagnosis.
- Polysomnogram (PSG): An overnight sleep study to rule out other sleep disorders.
- Multiple Sleep Latency Test (MSLT): A daytime nap study that measures how quickly a person falls asleep and enters REM sleep.
- CSF Hypocretin Level: A lumbar puncture (spinal tap) may be performed to measure hypocretin levels in the cerebrospinal fluid; low levels are a definitive marker for Type 1 Narcolepsy with cataplexy.
Differential Diagnosis
Cataplexy is often confused with other conditions that cause falls or loss of consciousness. It is distinct from fainting (syncope) because consciousness is preserved. It is also different from seizure disorders (epilepsy), specifically atonic seizures, as cataplexy is triggered by emotion and does not involve the post-event confusion typical of seizures. Doctors also rule out neuromuscular disorders and pseudoseizures.
Treatment and Management
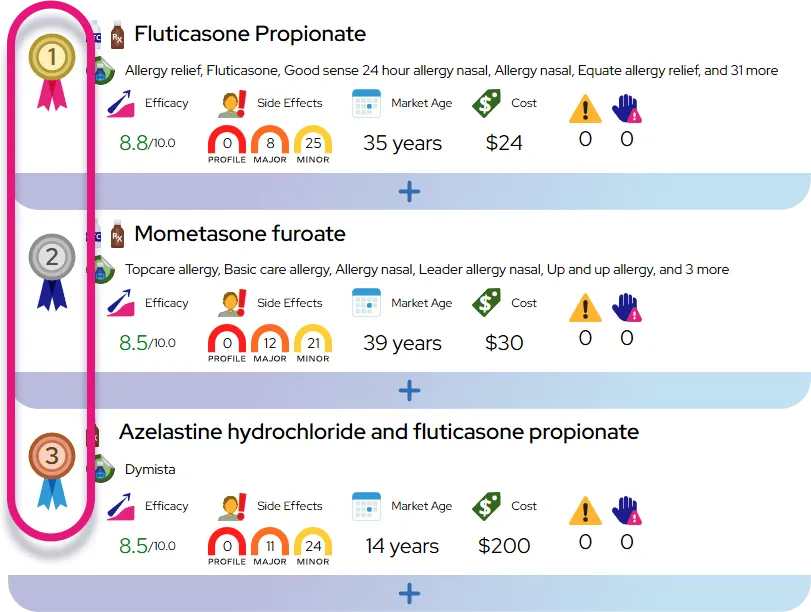
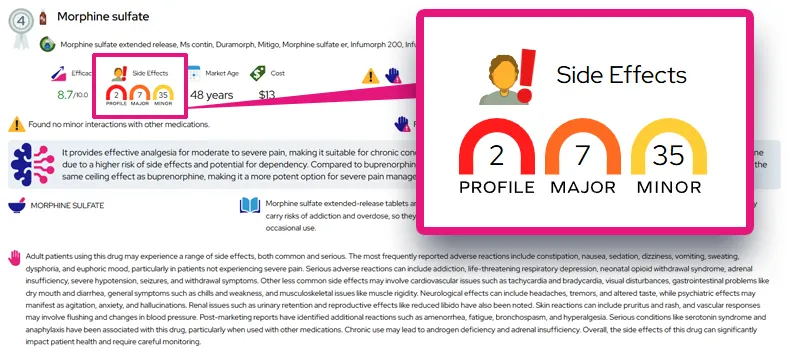
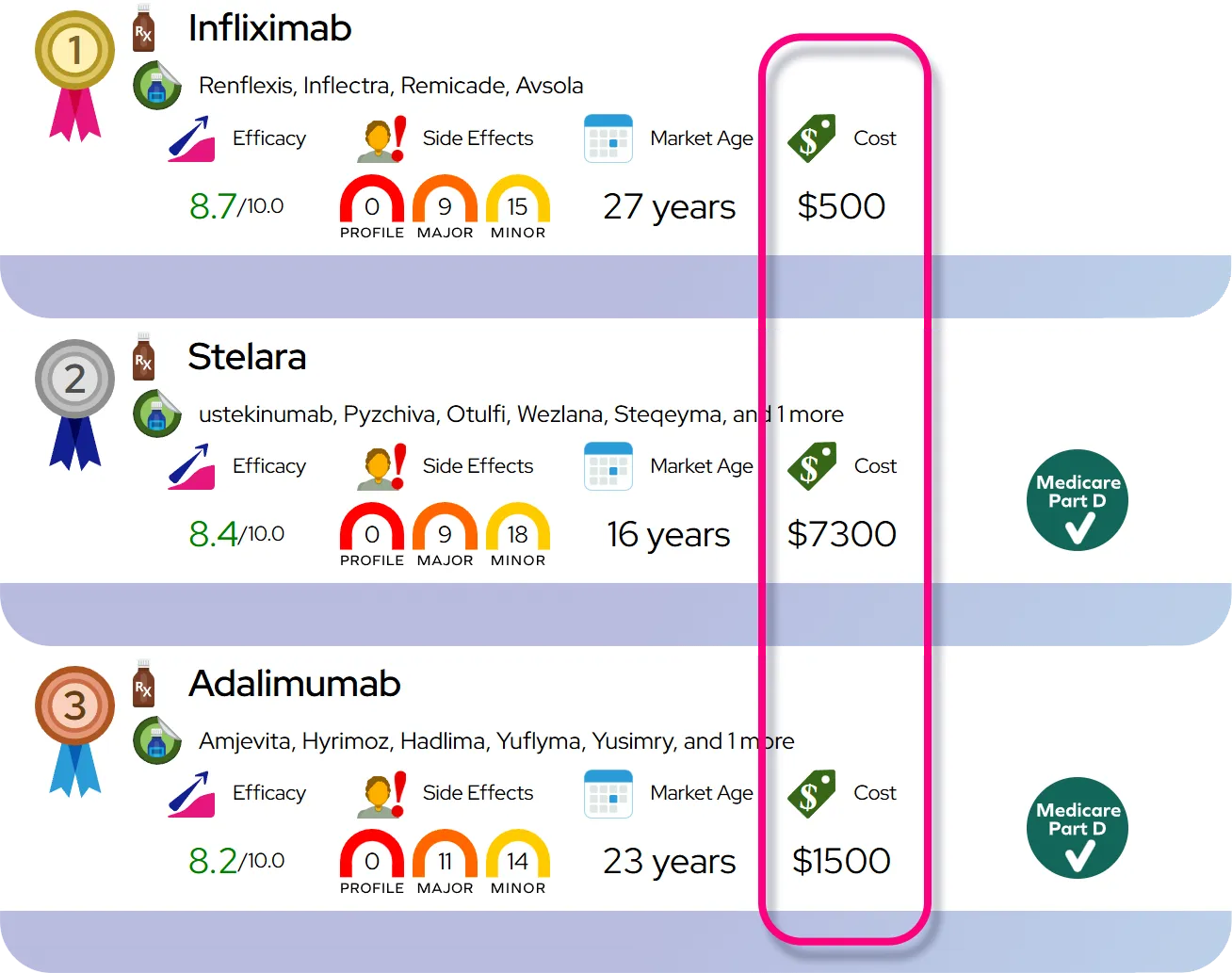
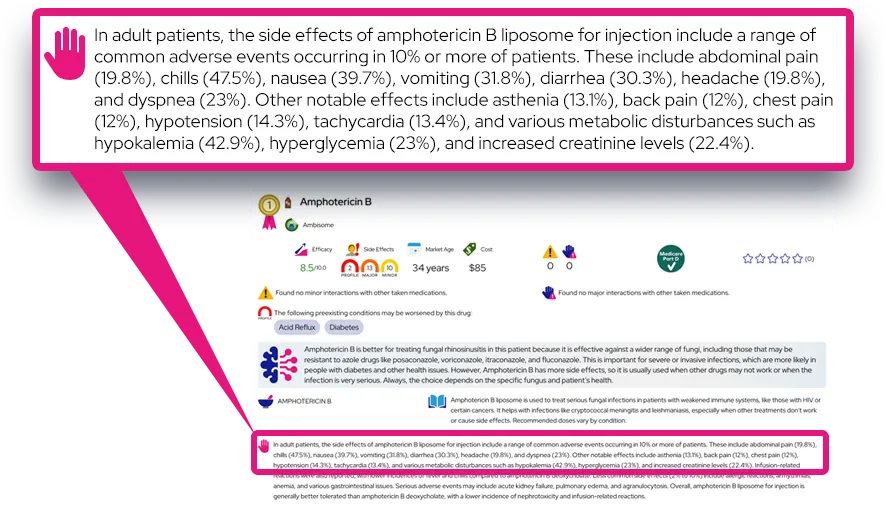
Medications
Treatment primarily focuses on symptom management using medications that suppress REM sleep or increase wakefulness chemicals in the brain. Sodium oxybate and similar oxybate salts are the only medications FDA-approved specifically to treat cataplexy and are highly effective for many patients. Antidepressants, such as Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), and Tricyclic Antidepressants, are often used off-label to suppress REM sleep and reduce attacks. Pitolisant, a histamine-acting medication, is also used to treat cataplexy.
Lifestyle and Self-Care
Managing lifestyle factors plays a crucial role in reducing the frequency and impact of attacks. While medication is the main line of defense, behavioral changes help maintain safety and stability.
- Sleep Hygiene: Maintaining a consistent sleep schedule and taking scheduled short naps can reduce overall fatigue, which often worsens symptoms.
- Safety Precautions: Patients may need to modify their environment, such as using plasticware instead of glass, or avoiding driving when symptoms are poorly controlled.
- Trigger Awareness: While avoiding emotions entirely is not healthy, being aware of high-risk situations (like a comedy club) allows patients to prepare by sitting down or having support nearby.
When to Seek Medical Care
Regular follow-up with a sleep specialist is essential to monitor medication effectiveness and side effects. Patients should seek immediate care if they suffer an injury from a fall during an attack. A doctor should be consulted if attacks become more frequent, last longer than usual, or if new symptoms emerge. If symptoms of depression or anxiety develop due to the condition, mental health support should be sought.
Severity and Prognosis
Severity
The severity of cataplexy varies widely among individuals. Some people experience only rare, mild episodes (such as knees buckling once a month), while others may have frequent, severe attacks (multiple daily collapses). Factors such as stress, poor sleep, and illness can temporarily worsen the severity. The condition is broadly classified based on the frequency of attacks and the degree of muscle loss.
Disease Course and Prognosis
Cataplexy is a chronic condition, but it is not progressive in the sense that it does not cause physical degeneration of muscles or nerves over time. In fact, for many patients, the frequency of attacks tends to decrease with age, and some may experience long periods of remission. However, without treatment, it can significantly disrupt daily life. Life expectancy is normal, and mortality is not directly associated with the condition itself, but rather with accidents that may occur during an episode (e.g., falling while driving or swimming).
Complications
The primary complications are physical injuries from falls, such as bruises, fractures, or head trauma. Long-term complications often involve the psychological impact, including social anxiety and withdrawal, as patients may avoid social interactions to prevent emotional triggers.
Impact on Daily Life
Impact on Daily Activities
Cataplexy can interfere with routine tasks such as cooking, driving, and working. Many patients may need to avoid jobs that require operating heavy machinery or working at heights. Driving is generally permitted only when the condition is well-controlled with medication and cleared by a physician. Simple adjustments, like sitting down when laughing or feeling excited, become second nature for many.
Emotional and Social Health
Because strong emotions trigger attacks, patients often develop a fear of expressing themselves. This can lead to "emotional blunting," where a person intentionally suppresses laughter or excitement to avoid embarrassment or injury. This suppression can result in social isolation, strained relationships, and increased risk of depression or anxiety. Support groups and counseling are vital resources.
Questions to Ask Your Healthcare Provider
Patients should feel empowered to discuss safety and quality of life with their doctor.
- Is it safe for me to drive, and what are the legal requirements in my state?
- What specific side effects should I watch for with my new medication?
- Are there any over-the-counter drugs I should avoid that might worsen my symptoms?
- How can I explain this condition to my employer or school to get accommodations?
- What should I do if I plan to become pregnant?
Common Questions and Answers
Q: Is cataplexy the same as a seizure?
A: No. While they can look similar, cataplexy is different because the person remains fully awake and aware of their surroundings, whereas seizures often involve a loss of consciousness or awareness.
Q: Can cataplexy happen while I am asleep?
A: No, by definition, cataplexy occurs while you are awake. However, it is related to the paralysis that naturally occurs during REM sleep, which is why it affects muscle tone.
Q: Will I swallow my tongue or stop breathing during an attack?
A: No. The muscles that control breathing and the diaphragm are not affected during an attack, so you will continue to breathe normally. It is not possible to swallow your tongue.
Q: Can cataplexy be cured?
A: There is currently no cure for the underlying cause (Type 1 Narcolepsy), but medications are very effective at reducing or eliminating the frequency of cataplexy attacks for most people.
Q: Does everyone with narcolepsy have cataplexy?
A: No. Narcolepsy is divided into two types. Type 1 includes cataplexy, while Type 2 does not. Cataplexy is the main distinguishing feature between the two types.