Actinic keratosis
At a Glance











How It Affects You
Actinic keratosis, also known as solar keratosis, manifests as rough, scaly patches on areas of the skin that have accumulated significant sun damage over many years. These growths are typically found on high-exposure sites, most notably the face, ears, scalp, neck, forearms, and the back of the hands.
- The lesions often feel like sandpaper and can range in color from skin-toned to reddish-brown.
- While they are primarily a cosmetic concern initially, they indicate cellular damage within the skin.
- If left untreated, these precancerous spots have the potential to progress into squamous cell carcinoma, a type of skin cancer.
Causes and Risk Factors
Underlying Causes
The primary cause of actinic keratosis is long-term exposure to ultraviolet (UV) radiation from the sun or tanning beds. This radiation damages the DNA within the skin's outer layer, specifically the keratinocytes. When the body cannot repair this damage effectively, the cells begin to grow and divide abnormally, resulting in the characteristic scaly lesions.
Risk Factors
Several factors significantly increase the likelihood of developing this condition. People with fair skin, red or blond hair, and blue or light-colored eyes are at the highest risk because they have less protective pigment. Additional risk factors include:
- A history of intense or frequent sun exposure and sunburns.
- Living in sunny climates or at high altitudes.
- Being older than 40 years of age.
- Having a weakened immune system due to medical conditions or organ transplant medications.
Prevention Strategies
Preventing actinic keratosis centers on protecting the skin from UV radiation. Primary prevention involves minimizing sun exposure during peak hours, usually between 10 a.m. and 2 p.m., and avoiding tanning beds entirely. Wearing protective clothing, such as wide-brimmed hats, long-sleeved shirts, and sunglasses, provides a physical barrier against UV rays. Consistent use of broad-spectrum sunscreen with an SPF of 30 or higher is crucial for exposed skin. While existing damage cannot always be reversed, these measures help prevent the formation of new lesions and reduce the risk of existing ones becoming cancerous.
Diagnosis, Signs, and Symptoms
Signs and Symptoms
Actinic keratosis typically appears as a rough, dry, or scaly patch of skin. These lesions are often felt before they are seen, frequently described as having a texture similar to sandpaper. They are usually small, ranging from the size of a pinhead to a quarter of an inch in diameter. Visually, they can vary in color, appearing pink, red, brown, or the same color as the surrounding skin. Some lesions may cause sensations such as itching, burning, or stinging, while others are asymptomatic. In some cases, a hard, horn-like growth known as a cutaneous horn may project from the skin.
Diagnosis
Healthcare providers typically diagnose actinic keratosis through a visual examination of the skin. A thorough inspection allows the clinician to identify characteristic features of the lesions. Sometimes, a dermatoscope—a specialized magnifying device—is used to examine the spot in greater detail. If a lesion looks suspicious, bleeds, is exceptionally thick, or does not respond to treatment, a skin biopsy may be performed. This involves removing a small sample of the tissue for microscopic analysis to confirm the diagnosis and rule out invasive cancer.
Differential Diagnosis
Actinic keratosis can resemble other skin conditions. It is often distinguished from seborrheic keratosis, which usually has a waxy, stuck-on appearance, and psoriasis, which typically presents with silvery scales. It must also be differentiated from basal cell carcinoma and squamous cell carcinoma, which are forms of skin cancer that may require more aggressive treatment.
Treatment and Management
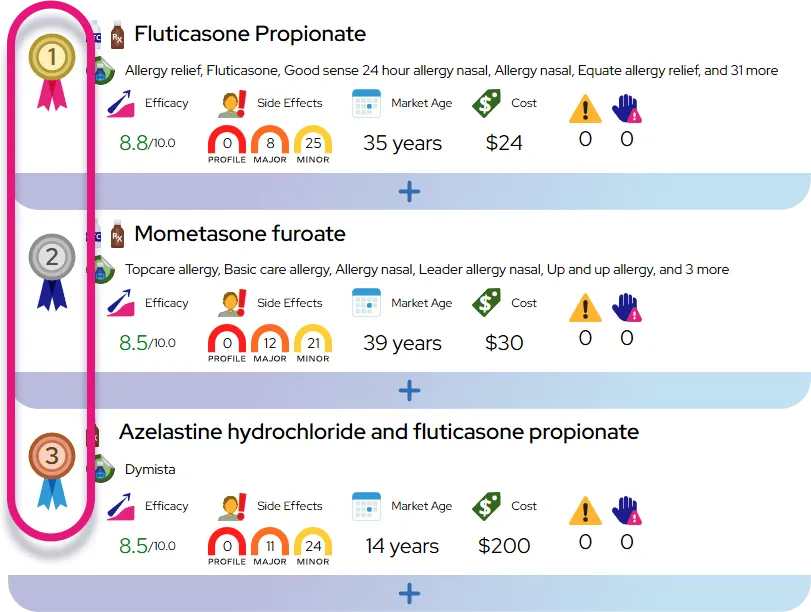
Medications and Topicals
Topical treatments are commonly used, especially when there are multiple lesions in one area, a concept known as field therapy. Creams or gels containing 5-fluorouracil (5-FU), imiquimod, tirbanibulin, or diclofenac are applied directly to the skin. These medications work by destroying abnormal skin cells or stimulating the local immune response. Patients typically experience temporary redness, peeling, and crusting as the skin heals, which is a sign that the treatment is working.
Procedures and Surgeries
For individual or thicker lesions, doctors often use procedural treatments. Cryotherapy is the most common method, involving the application of liquid nitrogen to freeze and destroy the lesion. As the treated area heals, the damaged skin falls off and is replaced by new skin. Other procedures include curettage and electrosurgery, where the lesion is scraped away and heat is used to stop bleeding. Photodynamic therapy (PDT) involves applying a light-sensitizing solution to the skin and then exposing it to a specific light to kill the precancerous cells.
Monitoring and Management
Since actinic keratosis indicates sun damage, patients are likely to develop more lesions over time. Regular self-exams and professional skin checks are essential for long-term management. Treating these lesions effectively prevents them from progressing to skin cancer. Lifestyle changes, particularly strict sun protection, are integral to managing the condition and preventing recurrence.
When to Seek Medical Care
You should see a doctor if you notice any changes in your skin that concern you. Specific reasons to seek care include:
- A spot that bleeds, oozes, or does not heal after a few weeks.
- A lesion that grows rapidly, changes shape, or changes color.
- The development of a hard, horn-like bump on the skin.
- Any new rough or scaly patches that persist.
Severity and Prognosis
Severity and Progression
Actinic keratosis is generally considered a mild to moderate condition in terms of immediate health impact, but it serves as a critical warning sign of cumulative sun damage. The severity is often judged by the number of lesions present and the extent of the affected area. While a single lesion is not dangerous, the presence of multiple lesions indicates "field cancerization," meaning a large area of skin has been damaged and is unstable.
Prognosis and Complications
The prognosis for treated actinic keratosis is excellent. Most lesions can be cleared completely with appropriate therapy. However, the primary risk associated with this condition is the potential for progression to squamous cell carcinoma (SCC), a type of invasive skin cancer. While the percentage of individual lesions that turn into cancer is relatively low, the majority of squamous cell carcinomas begin as actinic keratoses. Occasionally, lesions may disappear on their own, but they frequently recur. Long-term monitoring is necessary because the underlying sun damage persists, and new lesions are likely to develop over the patient's lifetime.
Impact on Daily Life
Impact on Daily Activities
Living with actinic keratosis generally does not limit physical activities, but it requires incorporating diligent sun protection into daily routines. This involves applying sunscreen every morning and reapplying it when outdoors, as well as wearing hats and protective clothing. Some treatments, particularly topical creams, can cause visible redness, scabbing, or peeling on the face or hands for several weeks. This temporary alteration in appearance may affect social confidence or require planning treatment around significant life events.
Emotional and Mental Health
A diagnosis of a precancerous condition can cause anxiety about the risk of developing skin cancer. However, knowing that the condition is treatable and that proactive management significantly reduces cancer risk can provide reassurance. Establishing a routine with a dermatologist helps manage this anxiety.
Questions to Ask Your Healthcare Provider
Being prepared for your appointment can help you understand your condition and treatment plan. Consider asking the following questions:
- What is the most effective treatment for the specific location and number of my lesions?
- How can I distinguish between a harmless spot and one that might be cancer?
- What side effects should I expect from the prescribed treatment, and how long will they last?
- How often do I need to return for a full-body skin exam?
- Are there specific sunscreen brands or skincare products you recommend for my skin type?
Common Questions and Answers
Q: Is actinic keratosis contagious?
A: No, actinic keratosis is caused by sun damage and cannot be spread from person to person through contact.
Q: Will every actinic keratosis turn into skin cancer?
A: No, most lesions do not turn into cancer. However, because it is difficult to predict which ones will progress to squamous cell carcinoma, doctors recommend treating them to minimize the risk.
Q: Can I just scratch the lesion off?
A: You should not attempt to scratch or pick off the lesions. This can cause bleeding, infection, and scarring, and it does not remove the abnormal cells deep in the skin, so the lesion will likely return.
Q: Does insurance typically cover treatment?
A: Yes, because actinic keratosis is a precancerous medical condition, treatment is generally covered by health insurance plans, unlike cosmetic procedures.
Q: Can actinic keratosis go away on its own?
A: Sometimes lesions may disappear, but they often reappear later. Because of the risk of cancer, it is safer to have them evaluated and treated rather than waiting for them to resolve.